Adenomas Of The Liver
Liver disease is serious and requires treatment and regular monitoring by a liver specialist.
A liver specialist is known as a hepatologist and you need to be referred by your family doctor or general practitioner. Over nearly 40 years of practicing medicine I have seen many patients develop severe liver disease, which sadly could have been prevented by early detection and early referral to a hepatologist. There needs to be more awareness of liver disease so that patients can be treated early so that we can prevent cirrhosis, liver failure and liver cancer. Make sure you have your liver function checked annually with a blood test.
I have presented my ideas on how to help those with liver diseases using nutritional medicine, which I have been using for many years with good success rates. However my recommendations do not replace the care of your own doctor and you should remain under the care of your own doctor whilst using nutritional therapies.
If you have any questions you may contact my naturopath, Christine, on 623 334 3232 or email us at support@liverdoctor.com
Adenomas of the liver
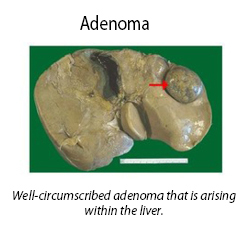
Liver cell adenoma is a common and benign (non-cancerous) tumor of the liver. A liver adenoma is an encapsulated liver tumor (has a capsule around it) and it does not contain bile ducts.
 Causes of liver adenomas
Causes of liver adenomas
Since the 1980s liver cell adenoma and liver cell adenomatosis (multiple adenomas) have emerged as new entities in medical practice due to the widespread use of oral contraceptives and high dose hormone replacement therapy.
The increased prevalence of patients with liver cell adenoma is due to the widespread use of estrogen-based oral contraceptives, as well as the increased use of imaging tests (such as ultrasound scans and CAT scans) of the abdomen for a variety of unrelated reasons. This means that many adenoma tumors are identified as incidental findings in patients with no liver symptoms. The clinical importance and natural history of these incidental adenoma tumors is not fully understood, and there is a need for optimal management strategies in such patients.
The causal relationship between oral contraceptives and other oral estrogens and liver cell adenoma is proportional to the dose and duration of the hormone medication. The incidence is highest in women over 30 years of age after using oral contraceptives for more than 2 years. It is estimated that the risk of growing an adenoma increases by a factor of 5 after 5 years, and by 25 after 9 years of oral contraceptive usage.
Outcome of liver adenomas
Liver adenoma has a low possibility of bleeding into the liver. Transformation into liver cancer is rare; however this risk goes up if the adenoma has a diameter of over 5 centimetres. Pregnancy often stimulates rapid growth in liver adenomas with risk of potentially fatal spontaneous rupture and such patients should be referred to a top liver specialist.
Diagnosis of liver adenoma
The best imaging technique is an MRI scan of the liver. If the adenoma is very large or looks suspicious for liver cancer, it can be biopsied for definite diagnosis.
Treatment of liver adenoma
If the patient is on oral contraceptives or estrogen containing hormone replacement therapy it is vital to cease using them. This often results in the adenoma shrinking and oral contraceptive-induced liver cell adenomas are reversible if oral contraceptives are discontinued within a certain time period. With prolonged oral contraceptive usage, pre-cancerous changes (dysplastic foci) may develop within the adenoma that may progress to liver cancer. The causative role of oral estrogen containing contraceptives in producing liver cell adenoma is beyond doubt, and many studies have shown regression and even complete disappearance of adenomas after cessation of the oral contraceptive pill.
Because adenoma has a risk of bleeding and malignant transformation, surgical excision is usually done for solitary liver adenomas.
Liver cell adenomatosis
Liver cell adenoma caused by estrogen ingestion is usually solitary (one tumor only), but some people may develop several adenomas spread throughout the liver. This latter condition is known as liver cell adenomatosis and does not have the strong association with estrogen or anabolic steroid use.
If the tumors are causing severe symptoms and are accessible to surgery, they should be surgically removed. Other treatments such as embolization (blocking the blood supply) to bleeding tumors and radiofrequency destruction may be useful in some patients.
Follow up
Regular and long term medical supervision is vital because even complete disappearance of the adenoma does not prevent the later development of liver cancer, which has been observed five years after cessation of oral contraceptive usage and regression of the adenoma.
There are no reports of new adenoma formation or development of liver cancer after surgical removal of solitary liver cell adenoma.
In liver cell adenomatosis where there is extensive distribution of the lesions, management decisions are more problematic, as targeted adenoma excision is not an easy treatment. If there are many large tumor nodules ranging from 1 to 4 inches (2–10 cm) in diameter, then enlargement and deformation of the liver may occur. This is called a “massive type” and may be rapidly progressive and presents a real treatment challenge. The ‘multifocal type’ contains many adenomas up to 2 inches (4-5 cms) in diameter but the liver shape is not deformed or enlarged. These patients are unlikely to have many symptoms and appear to have a less aggressive clinical course.
Patients should be entered into a follow up program that includes yearly CAT scans or MRI scans, and frequent serum alpha-fetoprotein (AFP) measurement in a blood test. AFP is a protein that is a marker for liver cancer and rising levels must be taken seriously. These tests are done to detect progression of disease (increased lesion size) and/or transformation into liver cancer.
All female patients should be advised to stop hormone medication (e.g. oral contraceptives and hormone replacement therapy), and also ensure that they prevent further pregnancies.
Those who have the massive form of liver cell adenomatosis may have multiple large lesions within a single lobe of the liver, and are best managed by partial removal of the liver. Patients with multifocal liver cell adenomatosis should be monitored with regular liver imaging. Progression of disease with larger adenomas, concern of malignant transformation, and increasing symptoms are indications for resection in multifocal liver cell adenomatosis. Resection is the preferable option unless technically impossible.
Liver transplantation should be considered only as a last resort. Indications where liver transplantation is considered may include rise in serum alpha-fetoprotein, concern about transformation to cancer on scans, and patients with marked enlargement of the liver and repeated bleeding of the adenomas.
Nutritional help for adenomas
In patients with liver adenomas, either solitary or multiple, it is important to have a healthy diet and to avoid eating sugar and refined carbohydrates. If you are overweight, a low carbohydrate diet that is free of all grains and refined sugar is important and may shrink tumors. This is because a low carbohydrate diet lowers insulin levels and insulin is a growth promoting hormone that can promote the growth of tumors.
It is vital to support healthy liver function to try and shrink the adenomas; I recommend the following –
- Selenomune
Take one capsule daily with food. Selenium has been studied in large clinical trials and has a proven effect in reducing liver cancer. Selenomune is the leading selenium supplement available and contains the correct dose.
- Vitamin D3
Especially if you are low in blood levels of vitamin D.
- Super Vitamin K
Take 2 capsules daily with food.
- N-Acetyl-Cysteine (NAC)
Take 1 capsule twice daily.
The above statements have not been evaluated by the FDA and are not intended to diagnose, treat or cure any disease.

 Causes of liver adenomas
Causes of liver adenomas
Leave A Comment